OCTOBER: The Multidisciplinary Approach to Pain
Multidisciplinary Treatment of Chronic Pain
Chronic pain has traditionally been defined as pain that persists for a period longer than 3 months. However, recent discoveries regarding the physiopathological mechanisms involved in the development of chronic pain have rendered the identification of pain chronicity based solely on its duration somewhat obsolete.
One of the fields that has contributed significantly to this redefinition of chronic pain is neuroscience. Research in this area has demonstrated structural and functional changes in the central nervous system of individuals suffering from chronic pain, which alter the processing of potentially harmful stimuli, thus facilitating the experience of pain. In other words, individuals with these processing alterations are more prone to experiencing pain than the rest of the population (Hashmi et al., 2013). Furthermore, in some cases, these alterations are sufficient on their own for individuals without any structural injuries to experience pain. This is why we now consider chronic pain to be those painful clinical conditions that persist beyond the tissue healing time, no longer being a symptom of structural injury but the pathology itself (Treede et al., 2019).
This prolonged experience of pain can affect the quality of life in ways that go beyond the pain itself. Depression, anxiety, chronic fatigue, and sleep disturbances are some of the most common comorbidities of chronic pain (Yalcin & Barrot, 2014; de la Vega et al., 2019). All of this makes the chronic pain patient a complex case, one that could benefit from a multidisciplinary approach.
Multidisciplinarity plays an essential role in addressing the person from a holistic perspective, caring for and attending to the different areas that can be affected by this condition. Pain management by a multidisciplinary team allows for an individualized intervention tailored to the needs of the person with chronic pain (Nahin, 2022). According to a recent study by Staudt et al. (2022), the primary professionals that make up the multidisciplinary pain management team include physiotherapists, anesthesiologists, nurses, psychologists, among others.
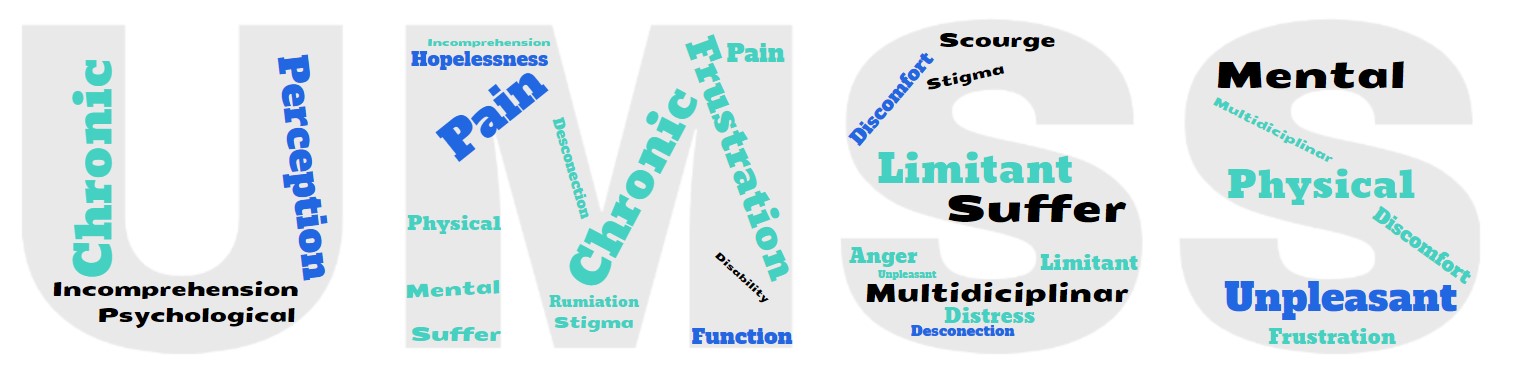
At UMSS, we have considered how professionals who may constitute the multidisciplinary team perceive chronic pain. Therefore, we asked a physiotherapist, an anesthesiologist, a nurse, a psychologist, and a pharmacist the following questions: How would you define chronic pain? Have you ever experienced chronic pain, and if so, how did it make you feel? In response to the question, “How would you define chronic pain?” all professionals integrated both the physical and psychological aspects into their definition, indicating that they all view both aspects as a unified concept in chronic pain.
“An aversive and alarm reaction experienced by an individual, involving both physiological and psychological mechanisms, with a high emotional component. Pain can be debilitating, especially when it is chronic and extends beyond its initial cause, interfering with a person’s daily life and functioning.”
“The physical perception of an unpleasant nature that limits a person’s normal activities from both a functional and psychological standpoint. Chronic pain often has a close association with musculoskeletal conditions.”
“Beyond being an unpleasant sensory experience, it is evident that chronic pain is more than that. It has a significant emotional impact that influences how you think and behave with yourself and in your environment. It is a challenge to get to know your body in a different state than usual, and where you learn to manage your body, emotions, and catastrophic thoughts.”
“Pain is not just a physical experience but also a form of suffering for the individual. It is not just an organic injury but vital for how the person lives and experiences pain emotionally, functionally, and in their overall quality of life.
“Chronic pain is an unpleasant perception that has two aspects, a physical and a psychological one. Pain from a physical perspective is that which is felt and has an organic or physiological cause, while the psychological aspect is sometimes experienced as a limitation, accompanied by self-stigma and associated labels that do not allow for the physical and emotional well-being of the individual.”
When asked whether they had ever experienced chronic pain, three out of the five respondents indicated that they had, with causes including herniated discs, chronic back pain, and migraines. In these cases, the various professionals who reported experiencing or currently experiencing chronic pain expressed feeling limited, frustrated, irritable, isolated from their surroundings.
“Pain limited me in terms of performing certain movements. I had to normalize not doing certain things in my life that were detrimental to me. When I experienced physical discomfort due to pain, it was accompanied by emotional distress because I felt very restricted, almost disabled by it.”
“Pain made me feel frustrated due to the extensive duration of symptoms, which sometimes seem like they will disappear, only to return even stronger. Another issue was the limitation in your daily activities, both at home and at work. Another problem is that it sometimes made me a bit more irritable with people in my surroundings.”
“Pain led me to experience a disconnection from my surroundings. For me, it’s a burden, a weight that results in attention deficit due to the presence of pain, often leading you to reject social activities due to the discomfort experienced, distancing you from your environment. You feel handicapped, and when you get used to it or cope with it, it becomes part of your life, but it’s like having a continuous hangover.”
The professionals who had not experienced chronic pain expressed how they had witnessed the experiences of others with chronic pain in their social or work environments.
“Pain can be incapacitating for the individual. Often, when there is no direct cause-effect relationship explaining that pain, the person feels misunderstood both by their social and work environment, as can happen in fibromyalgia. Ultimately, this only aggravates the problem.”
“The individuals I have worked with who have experienced chronic pain often feel frustrated by the conditioning of pain. Many of these individuals, through my work, have expressed feelings of hopelessness and distress. They also cannot help but ruminate, and pain occupies a significant portion of their daily thoughts.”
From the interviews with the various professionals, we can conclude that chronic pain is a comprehensive issue affecting the individual, including physically, psychologically, and socially. This underscores the importance of managing chronic pain with a multidisciplinary team, which we at UMSS aim to highlight and support through this blog entry.”